Spanish researchers use brain modeling to identify necessary circuits of consciousness
Currently, patients with DoC are classified into several categories (coma, unresponsive wakefulness syndrome, and minimally conscious state) which describe their overall consciousness and awareness. “The diagnosis is mainly response-based: the doctor sits down with the patient and assesses their response to stimuli” explains Jitka Annen from the University of Liège. “However, this may not correspond to their underlying brain activity - patients with high activity may still be unable to react. It’s a heterogeneous group. We wanted to go a step beyond assessment and classification based on neuroimaging and instead look at the flow of information in their brains, to find common patterns associated with consciousness.”
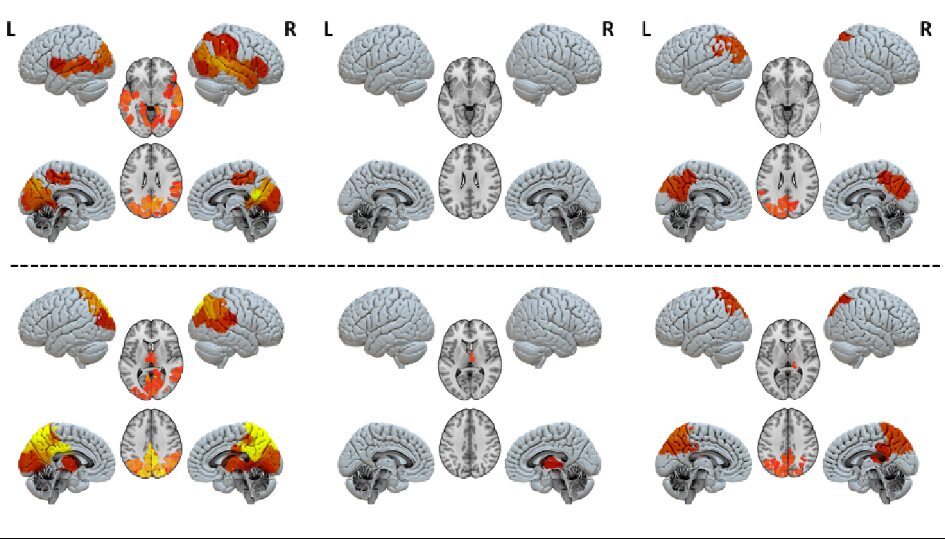
The researchers focused on two DoC groups - unresponsive wakefulness syndrome (previously known as the vegetative state) and the minimally conscious state. After collecting fMRI data from each patient during resting state (i.e., patients were awake but no particular task was provided), they looked at the spontaneous and model-based perturbation of brain activity captured by the blood flow, such as signals and peaks. “Based on spontaneous peaks of activity, we evaluated the personalized connectivity of each patient’s brain, which can tell us how likely a signal is to travel from one point to the other,” says Gorka Zamora-López from Pompeu Fabra. “After we constructed a patient-specific computational model of their propagation patterns, we then trigger a signal in the model and see how the brain reacts. In particular, we look for which areas are more likely to respond to a signal; which areas are more likely to propagate it. Basically, we look at whether an area acts as an influencer or influenced.”
A marked distinction arises between the unresponsive wakefulness syndrome group and the minimally conscious state group, with the former not displaying activity in identifiable circuits. “The key difference is that in patients with unresponsive wakefulness syndrome, no region of the brain seems embedded in a functional network, they all display equally low activation. Meanwhile, distinct regions and circuits pop out in the brain models of people in the minimally conscious state: the thalamic-frontotemporal region when broadcasting signals, and the posterior cortical region when receiving them,” adds Rajanikant Panda of the University of Liège.
These findings shed new light on disorders of consciousness and could lead to a more defined understanding of the mechanisms based on brain activity rather than behavioral responses. “I believe these results can potentially guide the clinicians to better understand what is going wrong in the information exchange and thus look for ways to reactivate those circuits” concludes Zamora-López.
 How to resolve AdBlock issue?
How to resolve AdBlock issue?